People with dementia are particularly vulnerable to COVID-19 because of their age, multimorbidity, and difficulties in maintaining physical distancing. Severity and mortality of COVID-19 increase with age, and with pre-existing illnesses such as hypertension and diabetes, so people with dementia are at particular risk.
COVID-19, dementia, and mortality
Dementia and Alzheimer’s disease was the most common pre-existing condition found among deaths involving COVID-19 and was involved in 12,869 deaths (25.6% of all deaths involving COVID-19) in March to June 2020. Office for National Statistics analysis of trends in non-COVID-19 deaths (2 May 2020 to 10 July 2020) compared to the five-year average showed a large rise in excess deaths not attributed to COVID-19 during the first wave of the pandemic, alongside the spike in COVID-19 deaths. These deaths were largely in older age groups and there was a large spike in deaths due to dementia and Alzheimer’s disease during the period from March to May.
Undiagnosed COVID-19 cases could help explain this rise, while the slow decline may indicate deaths due to dementia and Alzheimer’s disease are linked to longer-term changes, such as changes to practice in care homes to combat COVID-19. Deaths involving dementia and Alzheimer’s disease occurred above five-year average levels for adults aged under 65, however, deaths involving dementia and Alzheimer’s disease in people aged 65 years and over were not above five-year average levels for the same period.
People with dementia may be at increased risk of infection if they receive support for personal care. Care homes have been particularly affected by COVID-19 and lockdown measures (changes to routines or group activities, mask-wearing, restrictions on family visits) may cause distress in people with dementia. Dementia and Alzheimer’s disease was listed in over half of COVID-19 deaths in care home residents in wave one (deaths registered week ending 20 March 2020 to 12 September 2020) and just under half of COVID-19 deaths in wave two (deaths registered week ending 12 September 2020 to 2 April 2021).
The most common pre-existing conditions in COVID-19 deaths in non-care home residents during both waves were diabetes (males) and hypertensive diseases (females, 22.6%).
COVID-19, dementia, and mental health
COVID-19 and control measures affected some people with dementia and their carers, for example, stress from dealing with COVID-19 rules, anxiety caused by social isolation, lack of respite care and fear of catching COVID-19. A survey of 1,800 carers and people living with dementia by the Alzheimer’s Society found 41% of people who received a care and support package had had this reduced or stopped since lockdown began. 46% of people with dementia said lockdown had a negative impact on their mental health, and 95% of carers reported a negative impact on their own mental or physical health.
It has been suggested the impact of COVID-19 might lead to increased neuropsychiatric symptoms and use of psychotropic medication. The three CCGs that cover Suffolk had worse (higher) rates of people with dementia prescribed anti-psychotic medication in the six weeks up to the end of October 2020 (Table 1) compared to England.
Table 1: Dementia: Proportion of people with dementia prescribed anti-psychotic medication in the last six weeks, October 2020, Persons, All ages
| Indicator | Value (%) | Count | Compared to England |
|---|---|---|---|
| NHS Ipswich And East Suffolk CCG | 11.8% | 440 | worse |
| NHS West Suffolk CCG | 12.5% | 295 | worse |
| NHS Norfolk & Waveney CCG | 13.8% | 1,396 | worse |
| England | 10.1% | 44,457 | does not apply |
Source: Public Health England Fingertips Dementia Profile
COVID-19 impact on diagnoses and service provision
COVID-19 and the measures put in place to reduce transmission have affected services supporting people with dementia, and collection of data used in reports like this. For example, data submissions for dementia assessment and referral were suspended for April 2020, and no data collection has been required for months up to and including July 2021 (date of this report).
A timely diagnosis of dementia relies on business as usual occurring in the health system, in particular access to a GP, as well as specialist services. Since March 2020, the COVID-19 pandemic has reduced business-as-usual health services in England, which “will have a significant impact on the quality of life for people living with dementia and their carers along with overall health outcomes”. For example, although Public Health England state “it is not possible to quantify the impact at this time”, data on the Estimated Dementia Diagnosis Rate in people aged 65 and over (EDDR) up to and including May 2021 shows:
- The EDDRs for May 2021 for Ipswich and East Suffolk CCG (59.2%), and West Suffolk CCG (59.5%) are similar to the England rate, but the EDDR for Norfolk and Waveney CCG (55.4%) is significantly lower.
- Ipswich and East Suffolk CCG and Norfolk and Waveney CCG have rates significantly lower than May 2019, although the West Suffolk CCG rate is 59.5%, similar to May 2019.
- The decrease in EDDR since May 2019 was greater than the England decrease (9.6%) in Ipswich and East Suffolk CCG (12.2%) and Norfolk and Waveney CCG (13.1%). The decrease in West Suffolk CCG was less (6.1%).
The proportion of people aged 65 and over with a formal diagnosis of dementia (prevalence) has decreased significantly in each of the three CCGs compared to May 2019 (3.9% Ipswich and East Suffolk CCG, 3.8% West Suffolk CCG, 3.6% Norfolk and Waveney CCG). The decrease in Ipswich and East Suffolk (12%) and Norfolk and Waveney (13%) is greater than the England decrease of 9.9%.
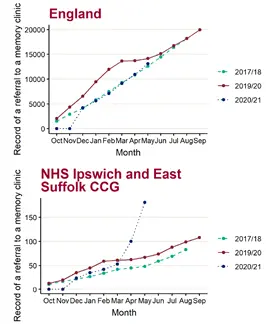
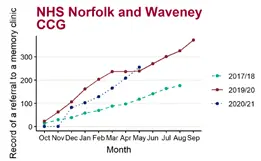
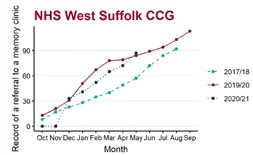
Most formal diagnoses of dementia are provided by specialist clinicians at memory assessment services (memory clinics). To receive a referral to a memory assessment service from primary care, an individual should be assessed by a general practitioner. Comparing cumulative counts of referrals to a memory clinic over the past three years shows (Figure 1, Figure 2, Figure 3):
- In May 2021, the number of people referred to a memory clinic aged 65 and over was higher in all the CCGs that cover Suffolk than May 2018: Ipswich and East Suffolk CCG (181), West Suffolk CCG (87), NHS Norfolk and Waveney CCG (255)
- The greatest increase in referrals since May 2018 was 277.1% in Ipswich and East Suffolk CCG, (52.6% West Suffolk CCG, 116.1% Norfolk and Waveney CCG, 3.8% England)
Note: The year starting October 2017 and ending in August 2018 has been used as a baseline as opposed to more recent years due to poor data quality. The 2017/18 baseline data is missing a point for September.
Source: Fingertips dementia profile report Wider impact of Covid19 on health – dementia surveillance factsheet (May 2021)